The Role of Belief in Health and Healing
Jan 10th 2023
(Somatic Movement Center) Belief is a powerful thing. In a 2001 study, researchers told a group of Parkinson’s patients that they were receiving a highly effective new drug that would improve their motor symptoms. However, the patients only received an injection of saline. Half of the patients experienced improvement in their motor systems because the damaged nigrostriatal dopamine system in their brains actually started producing more dopamine—up to 200% more in some cases—simply because they believed they were receiving an effective medication.
In a study of 180 patients with osteoarthritis of the knee, sham surgery proved to be equally as effective at relieving pain as two different types of real knee surgery (debridement and arthroscopic lavage). Over the course of the two years following the surgeries, the three groups of patients reported the same levels of pain relief. This outcome led the researchers to wonder if the money spent on these types of surgeries could be better spent elsewhere.
In 2016, researchers did a meta-analysis of studies that tested the efficacy of beta-blockers for treating high blood pressure. After analyzing 23 studies that included 11,067 participants, they found that “blood pressure was lowered in placebo groups with significant and robust effect sizes.” While hypertension is often treated with medication, the researchers concluded that “in light of these strong placebo responses, placebo mechanisms need to be considered in order to improve antihypertensive treatment.”
The placebo effect is often dismissed as being irrelevant to health and healing. How often have we ourselves said “It’s just the placebo effect?”
But, the results of the placebo effect—more accurately called the perception or belief effect, according to Dr. Bruce Lipton—are quite real, and that’s why some clinical trials compare treatments to placebos. Belief is such a powerful healer that pharmaceutical companies must prove that their medication works better than placebo in order to receive FDA approval.
Much of medical history is based on the placebo effect. Before the mid-20th century, medicine was not tightly regulated and few treatments were tested in clinical trials. The most important aspect of many treatments was that they gave the patient something to believe in. So, treatments that seem odd to us today became widely used for certain ailments, and whether or not the actual treatment was effective was fairly irrelevant; people believed that it was going to work, so it often did.
Back then, scientists didn’t understand on a cellular level why belief healed people. Now they do, and this knowledge is allowing us to understand why people with positive attitudes live longer, have better overall health, and can even heal from “incurable” diseases.
Yale University surgeon Bernie Siegel analyzed why some of his cancer patients with poor prognoses survived, while others with better prognoses died. He concluded that there are no incurable diseases, only incurable patients. This idea puts a tremendous amount of responsibility in patients’ hands—especially in a world in which we’ve been raised to trust doctors to make decisions about our health, rather than to trust ourselves.
As Dr. Joe Dispenza writes in his book You Are the Placebo, a doctor’s diagnosis is a modern-day voodoo curse. When a doctor tells a patient that their condition is incurable, the patients whose health tends to decline are the ones who accept their prognoses as fact. But the people who end up healing themselves and recovering from their incurable condition are the ones who do not accept their prognoses. They expect to get better, so they often do.
Unfortunately, the nocebo effect—believing that an outcome will be bad—is just as powerful. There is the much-cited case of Sam Londe, a retired shoe salesman who was diagnosed with esophageal cancer. He passed away soon after his diagnosis, but his autopsy revealed no trace of esophageal cancer. There were just a few small spots of cancer on his liver and lung, but not nearly enough to have killed him. His doctor, Clifton Meador, worried that his diagnosis had removed hope, and the case haunted him for decades afterward.
Many clinical trials find that people who receive the placebo experience some of the same side effects as the participants who receive the actual drug. A meta-analysis of 12 trials of the COVID vaccine, which included 45,000 people, found that up to three-quarters of the negative side effects of the vaccine can be attributed to the nocebo effect. Researchers told the participants that they might experience certain side effects like fever, headache, and fatigue, and so they did. More than 35% of participants who received a placebo reported these negative side effects, compared to just 46% of those in active vaccine groups.
In this post, I’ll discuss:
- Taking control of our genetics
- How belief affects our health at the cellular level
- How we reprogram our DNA and our cell’s receptors
- How we reprogram our neural circuitry
- How belief affects the immune system
Taking control of our genetics
In the wake of the Human Genome Project, we like to blame health conditions on predetermined genetics; we’re always looking for the specific gene that’s active in the majority of people who have a certain disease. But in reality, only about 2% of diseases can be blamed on single genes and can be considered truly unavoidable. The vast majority of us are born with genetics that can allow us to be healthy throughout our lives—given the right environmental conditions.
There are indeed genes that are correlated with many health conditions, but the science of epigenetics has proven that it’s the environment that determines whether or not these genes get expressed or suppressed. According to epigenetics expert Dr. Kenneth Pelletier, author of Change Your Genes, Change Your Life, research shows that only 5% of an adult’s genes are unchangeable; the other 95% can be turned on and off by environmental factors.
What exactly is the “environment?” The environment that affects our genes includes factors outside our body that we may have limited control over, and inside our body that we potentially have total control over. Environmental factors that we have less control over include exposure to toxins, pesticides, pollutants, viruses, bacteria, mold, and climate. Some of these, depending on where we live, may be completely unavoidable or very difficult to avoid.
Environmental factors that we can have total control over include the food and drinks we consume, how much and what type of exercise we do, the medications we take, our stress level, how much sleep we get, and yes—even our thoughts, feelings, and beliefs.
Genes do not randomly turn themselves on and off. The majority of genes are inactive until an environmental signal tells them to turn on. And once they’re turned on, they require an environmental signal in order to be turned off.
Knowing that we have this tremendous power to determine which of our genes get expressed, and ultimately determine our health, is incredibly empowering and motivating. Here are some examples:
A 2008 study of men with prostate cancer tested the effects of an intensive nutrition and lifestyle intervention on the activity of their genes. The changes in their diet and lifestyle resulted in switching the activity of over 500 genes in just 90 days. Forty-eight genes were up-regulated (turned on) and 453 genes were down-regulated (turned off). Many of the gene switches significantly changed the biological processes that had caused the cancer in the first place, including tumorigenesis and protein metabolism and modification.
Studies of telomeres (protective endcaps on chromosomes that determine cellular aging) found that pessimism and perceived stress both have negative effects. One study found that “women with the highest levels of perceived stress have telomeres shorter on average by the equivalent of at least one decade of additional aging compared to low stress women.” Another study found that pessimism was independently associated with shorter telomere length, as well as a weaker immune system.
And a 2013 study of slightly overweight, sedentary men found that by exercising just twice a week for six months, the men altered the activity of 7000 genes—that’s almost 30% of the total human genome.
Even more incredible is the fact that when we change our genetic activity, we can pass those changes on to our children. In fact, a study of mice showed that genetic changes were present at least four generations later!
How belief affects our health at the cellular level
A thought is an electrochemical reaction. The approximately 100 billion neurons in our brain communicate with each other by sending electrical signals. Chemical neurotransmitters are released at each synapse (connection between neurons) to allow for the transmission of the electrical signal to the next neuron.
Every time we think a thought, our brain also makes a protein called a neuropeptide. Neuropeptides send messages to our body, which then has a corresponding emotion. This is why neuropeptides are referred to as Molecules of Emotion.
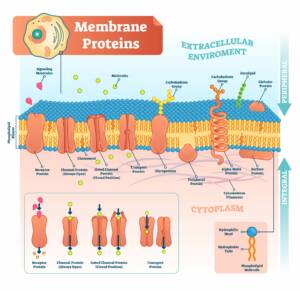
The outer layer of every cell in our body is called the cell membrane. To us it looks like the cell’s skin, but it actually operates as the cell’s nervous system.
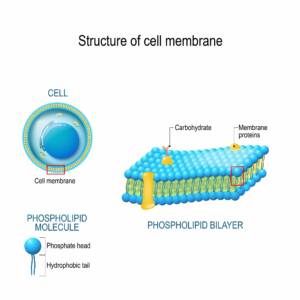
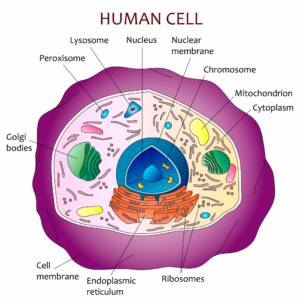
There are thousands of receptors that extend both inward and outward from the cell’s membrane. Some of these receptors respond to physical signals, like neuropeptides and hormones, and others respond to energetic signals like light, sound, and radio frequencies. The input that the receptors receive affects the behavior and structure of the cell. So as we have thoughts and experience emotions, the activity and structure of the trillions of cells throughout our body are affected.
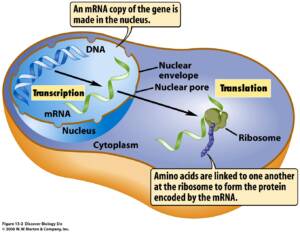
Within the nucleus of the cell lies the cell’s DNA. Regulatory proteins surround the DNA like a protective sleeve, preventing the DNA from being read. The only way to remove that sleeve of proteins is with—you guessed it—an environmental signal. When a signal from the environment triggers the protein sleeve to change shape and detach from the DNA, the DNA is exposed. A regulatory protein reads the genetic information, and RNA (ribonucleic acid, which acts as a messenger carrying instructions from DNA for controlling the synthesis of proteins) is produced. The RNA then exits the nucleus of the cell. The gene is now active and has the potential to affect your health.
One class of genes, known as IEGs (immediate early genes), takes only seconds to reach full expression once they’re turned on. IEGs often control the expression of hundreds of genes and thousands of proteins throughout the body. The fact that these genes can be switched on and off so rapidly could potentially explain cases of fast, miraculous healing that seem implausible.
The important takeaway from this is that the whole sequence of events starts outside the cell with the signal being sent from the environment. Genes don’t get expressed unless the environment tells them to be expressed. So when we take control of our environment, by consciously choosing our beliefs and how we live our daily lives, we take control of our cellular health.
This can be clearly seen in simple scientific experiments. When cells are put into an optimal growth medium in a petri dish, the cells thrive. When the same cells are put into a suboptimal growth medium, they become weak and die.
Reprogramming our DNA and our cell’s receptors
We’ve learned that environmental signals change the activity and structure of cells, including which genes within the nucleus are active. Repeated environmental signals also affect the receptors in the cell membrane.
Each receptor in a cell’s membrane is specific to one type of stimuli, like a neuropeptide, a hormone, or sunlight. When a cell is exposed to certain stimuli more often than others, it makes more receptors for the stimuli it’s exposed to most often. Cells also adapt by reducing the number of receptors for stimuli they’re exposed to less often.
This process of conditioning causes us to crave even more of the stimuli that we expose our cells to often. In this way, the body can control the mind, and we can become addicted to certain stimuli. And since every thought and emotion have corresponding neuropeptides that travel to our cells, we don’t just crave things like sugar—we crave things like habitual thoughts and emotions.
When cells divide in mitosis, the new cells that are produced have the same genetic activity and the same number and type of receptors. This is one of the ways in which we can change our biology: through the gradual process of cell programming and cell division. Cells divide and are replaced at varying rates throughout our body. As one cell divides and becomes two cells, we now have twice as many cells of that type—with the genetic activity and number and type of receptors that we’ve programmed it to have.
Reprogramming our neural circuitry
If we want to use positive thinking to change the cells in our body, we must first change the thoughts and beliefs that create the electrochemical messages and neuropeptides being sent to our cells.
As we learned, neuropeptides are called molecules of emotion because they trigger us to feel an associated emotion. There are more than 100 neuropeptide that have been discovered so far, and each one is associated with certain emotions, behaviors, and physiological activities.
When a neuropeptide triggers us to feel an emotion, our brain notices. This stimulates another thought that is closely matched to the emotion we’re feeling, which triggers the release of more of the same neuropeptide. Unless we consciously intervene, this cycle repeats over and over. Our thoughts and the corresponding emotions keep us stuck in a pattern of thinking and feeling a certain way. The more often the neurons involved in this pattern fire in the same pattern, the more deeply learned the pattern becomes—keeping us stuck in a fixed way of thinking and feeling.
Remember, our genes are turned on and off by our environment, which includes our thoughts, beliefs, and corresponding emotions. So as our hardwired neural patterns send the same neuropeptides to our body each day, the same genes are expressed, keeping us stuck in the same state of health. The only way to change which genes are expressed is to change the environmental signals being sent to our cells.
Studies show that 40 to 95 percent of our thoughts, emotions, and behavior are habitual—same as the day before, and the day before that. These habitual ways of thinking, feeling, and acting are controlled by our subconscious mind. Experts agree that our subconscious mind has a much greater effect on our health than our conscious mind.
So the big question is: How do we reprogram our subconscious mind to think more positive thoughts and send more positive signals to our body? We apply the principles of self-directed neuroplasticity, a phrase coined by Dr. Jeffrey Schwartz, which describes the act of consciously and intentionally changing your brain activities.
There are many ways to stimulate and direct positive changes in your brain activity, but the key to making those changes last is repetition. The older we get, the more hardwired our brain activities become, and the more practice and repetition it takes to override our deeply learned neural programs.
Some ways you can reprogram your habitual thoughts, beliefs, and emotions are:
- Repetitive positive thinking
- Allowing yourself to feel the emotion associated with the positive outcome that you desire
- Meditation
- Getting yourself into new environments, trying new experiences, and doing daily activities in new ways
- Visualization and mental rehearsal
- Hypnosis
- Cognitive Behavioral Therapy
- Body-centered therapies
There are many books, therapies, and different approaches that allow you to reprogram your subconscious mind. Two books that may be helpful to start with are Breaking the Habit of Being Yourself by Dr. Joe Dispenza and The Mind and the Brain by Dr. Jeffrey Schwartz.
How belief affects the immune system
The immune system is how our body heals from injuries, fights off foreign invaders, and protects against internal threats. When our immune system is not functioning optimally, we can succumb to viral and bacterial infections, autoimmune diseases, and cancer.
Many miraculous or unexplained instances of healing can be attributed to the immune system kicking into gear in response to a signal from the environment. One example is Anita Moorjani’s story, which she tells in her inspirational book Dying to be Me. On the brink of death, with cancerous tumors growing throughout her body and her organs shutting down, Anita had an out-of-body experience. She knew that if she chose to live, that she would experience a full recovery. When she awoke after being in a coma for 30 hours, her organs had begun to function again. Over the coming weeks, her tumors completely disappeared.
Studies consistently show how positive emotions and expectations improve immune function. A 2014 study of older adults showed that those who tended to have positive memories had stronger immune function than those who tended to have more negative memories.
An interesting study of mice showed how positive expectations that result in the clinical benefits of the placebo effect are mediated by the brain’s reward system. When the mice’s reward system was stimulated, they were better able to fight off a bacterial infection.
And a 2007 study carried out by scientists in Japan found that laughter improves immune function. After watching a funny video and laughing with hospital staff, test subjects had up-regulated 39 genes, 14 of which were related to natural killer cell activity.
Communication between the brain and the immune system is critical to our health. Current scientific evidence indicates that the neuroendocrine system (the hypothalamus-pituitary-adrenal axis) is the most powerful regulator of the immune system. The neuropeptides released in this axis stimulate hormones that regulate the immune system, and also act on the central nervous system which generates immunoregulatory nerve impulses. These neuroimmune mechanisms play an essential role in maintaining healthy immune function, and when they aren’t working properly, it can set the stage for autoimmune disease, chronic inflammation, and more.
We’ve learned how thoughts and emotions can cause genes to be expressed or suppressed. These epigenetic modifications can affect both our innate and adaptive immune responses. And now scientists are developing therapeutic approaches for certain diseases, such as cancer, that utilize epigenetic changes to strengthen the immune system and improve the efficacy of conventional treatments.
Chronic stress, while different than simply having negative emotions, can often lead to a pessimistic attitude and negative expectations. In a 2005 study, wounds of stressed patients took 40% longer than normal to heal, and the stressed patients had decreased levels of growth hormone at their wound sites. The stressed subjects expressed genes that encoded proteins responsible for cell cycle arrest, death, and inflammation. Another study found that people suffering from PTSD had six to seven times more epigenetic variations, most of which involved weakening the immune system.
Studies also show how stress makes it more difficult for us to fight off viral infections, including HIV and COVID-19. A 2001 study at UCLA found that HIV spread more quickly in patients who had higher levels of stress, and that stress made them less much less responsive to antiretroviral medications. Chronic stress, anxiety, and depression increase the risk of getting COVID-19 and having severe symptoms, and also increase the risk of having long COVID.
It’s important to remember that chronic stress can lie beneath the surface; it’s easy to adapt to an increased level of stress. We can be unaware that our subconscious mind is hyper-vigilant and constantly stimulating the release of stress hormones to our body, weakening our immune system.
In The Biology of Belief, Dr. Bruce Lipton reminds us that avoiding or eliminating negative stress only brings us to neutral. To be optimally healthy and “fully thrive, we must actively seek joyful, loving, fulfilling lives that stimulate growth processes.”
Research shows that activating the relaxation response with just one session of meditation immediately triggers expression of genes involving immune function, energy metabolism, and insulin secretion, and suppresses genes involved in inflammation and stress. Similarly, eight hours of mindfulness meditation reduces levels of proinflammatory genes and causes epigenetic changes that are associated with faster physical recovery from stressful situations.
And a 2008 study found that after practicing meditation and mind-body practices for eight weeks, participants upregulated 874 genes that promote good health and downregulated 687 genes that are involved in the stress response.
How to learn more
If you’re interested in learning more about how belief affects your health, I recommend reading The Biology of Belief by Dr. Bruce Lipton or You Are the Placebo by Dr. Joe Dispenza.
The Biology of Belief is an entertaining read about cell biology and includes discussion of how energetic forces, including thoughts, affect cellular behavior. You Are the Placebo offers more direct inspiration on how to use your thoughts and beliefs to change your health.
And if you are suffering from any health condition, always ask yourself: What in my internal or external environment could have contributed to this condition? What can I change or take control of?
Recommended reading:
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna